How much Vitamin D should we take?
It is as well to go back to the beginning.
Emergence of rickets
Rickest was perhaps the first disease of industrial civilisation.
During the 19th century it was clear that the childhood bone disease rickets was very rare, probably unknown, in the coastal communities of Scotland and the mountain communities of Austria, but it became increasingly common in the industrial cities. It was realised that the heavily polluted atmosphere was the cause, but what could be the treatment? Going to live in the mountains of Austria was not a realistic proposition for those living in cities. Similarly the population of Glasgow could not relocate to the coast.
So it was important to identify the factors of living on the coast, or in the mountains, that could somehow be brought to the populations of the cities. In Austria, children affected with rickets and tuberculosis (they often co-existed) had go to mountain fresh air, and as it turned out, the Sun shining out of clear air.
In the coastal communities of Scotland, cod liver oil was the answer. The fact that its active ingredient was unknown was not important: empiricalism was fine. It was obvious from observation and experience that cod liver oil could heal rickets and improve health. No more information was required. There had been no 'Randomised Controlled Trials', but large numbers of informal observations. The dose was ill-defined, just a spoonful a day.
The important thing is that in both Scotland and Austria it was agreed that the cause of rickets was atmospheric pollurion and indoor work, with little exposure to the sun..
Identification of Vitamin D
It was in the early 20th century that chemistry advanced to allow an analysis of cod liver oil, extracting the active ingredient. It was tested using laboratory mice. The amount of Vitamin D was so tiny that it could not be weighed and so it had to be measured by its biological effect. This was not easy and there had to be an international standard that would be equivalent to defined weights. It was decided and accepted that one unit of Vitamin D was the amount that was necessary for the optimal growth and apparent health of a ten gram immature mouse. Because it was accepted by all, it was called an International Unit, iu.
It was much later that it became possible to measure Vitamin D by weight. The mass of one unit was found to be 20 billionths of a gram, a very tiny amount.
We can scale up from the mouse. If one unit is the requirement of a ten gram mouse, a sixty kilogram human would require about 6,000 units.
This is a good starting point. Basing the dose of a Vitamin D supplement on body weight is sensible, 100 units per kilogram per day.
Recomendations from the UK Standing Committee on Nutrition (SACN) tells us that the recomended dose of vitamin D supplement is 400 units each day. This is based on the need to avoid rickets in children. Bone health is a steady state process, very different from escalation of defensive immunity. SACN only suggests that Vitamin D might have a role in immunity but is hardly convinced of this. Perhaps in the interests of caution, half the mouse equivalent dose might be adequate, 3,000 units each day for a 60kg person, 5,000 units each day for a 100kg person.
The need for monitoring and adjustment of dose
There is obviously variation in the need for individuals and so follow up assessment is necessary..
It is the same with insulin (discovered in 1922). The starting point for the dose is one unit per hour, the amount normally produced by the body. Once again insulin, identified at about the same time as Vitamin D, is measured in bilogical units, still maintained even though insulin can now be measured by mass.
For convenience and because of the short half-life of insulin, 24 units per day is usually given as 8 units three times a day, or 16 units in the morning and 8 units in the late afternoon.
Adjustments are made to meet the requirement of the individual as monitored by blood testing of blood glucose or HbA1c. There is no value in monitoring the blood levels of insulin as the effect of insulin is so variable. Type 2 diabetes is mainly due to insulin resistance, something not well-understood but which reduces the effect of insulin. In Type 2 diabetes blood levels of insulin are usually increased in that we are dealing with resistance not deficiency. The body's production of insulin increases in an attempt to overcome resistance, but the maximum production can be reached before this occurs and so diabetes develops.
There is also a variation of effect of Vitamin D, but this is quite rare and results from genetic variations in the structure of the Vitamin D Receptor, VDR polymorphisms. The way to assess routinely the appropriate dose of Vitamin D is to measure the amount of it circulating in the blood. But in doing so we do not measure, cholecalciferol, Vitamin D itself.
Vitamin D within the body
Most of our Vitamin D is produced in the skin by the action of UV from the sun on the oil 7-dehydro-cholesterol (7-DHC) that is synthesised in the skin (exceptin the very elderly.
When Vitamin D is produced in the skin, taken by mouth, or given by injection, it is taken in the blood to the liver. It then undergoes a slow conversion (by the addition of an -OH group) to 25(OH)D, also known as Calcidiol or Calcifediol. This is the important form of Vitamin D which is the reserve circulating in the blood, like petrol or deisel in the fuel tank of a car, or charge in a battery.
 |
Figure 1, Pathway of Vitamin D activation and action |
25(OH)D, a simple and accurate term, is carried in the blood bound to specific protein, called of course D-binding protein (DBP).
Genetic variations – polymorphisms
LIke all proteins DBP is synthesised in the body from a template that is genetically encoded. It is in our genes, and with all genes mutations (chemical errors) can occur. When mutations are compatible with life they can become a variation within the species. They are then called 'polymorphisms', different forms. But they might still give a disadvantage, and of course mutations are millions of times more likely to give a disadvantage rather than an advantage. In the reasonably well recorded history of humankind during more than two millenia, has there been a single advantageous mutation? There have certainly been millions of mutations that have been incompatible with life or causing serious disadvantage.
If there is a DBP polymorphism, the blood level of Vitamin D measured in its circulating form of 25(OH)D will not be able to give an accurate assment of Vitamin D status, causing the blood level to be inevitably deficient. This is however rare but is likely to encountered by a Vitamin D clinical specialist.
In practice the blood level of VItamin D as 25(OH)D is used as a measure of Vitamin D status, determining whether an individual is or is not deficient. It is also used to determine the appropriate dose of a supplement to correct Vitamin D deficiency.
'Ideal' or 'normal'?
In the treatment of diabetes, or thyroid disorder (over- or under-activity), or hypertension, or body weight, we do not just give a single dose of a tablet or injection, or diet to all, but we define an ideal target. We aim at an ideal blood glucose or HbA1c, or T4 and TSH, or blood pressure, or body weight. And so it is with Vitamin D. With all the ideal is identified by careful clinical observation.
It is better to use the term 'ideal' rather than 'normal'. 'Normal' is based on an average with the population distributed reasonably evenly on both sides of the average. But if most people are obese there will be a skew, and average 'normal' weight will be excessive, not ideal. We must aim for 'ideal', that which gives the greatest health advantage.
The extent of VItamin D deficiency
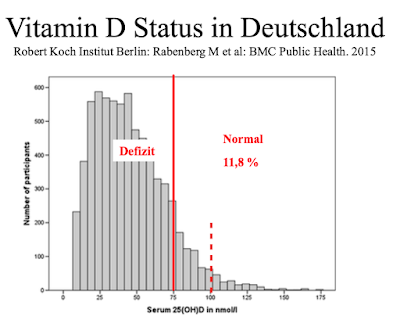
Most people have blood levels of Vitamin D that puts them at a disadvantage. The has been shown in many studies before and during the Covid-19 pandemic. An example is a population survey in Germany in 2015.
 |
| Figure 2. Vitamin D status in Germany |
We can see in Figure 2 the result of a population sample study undertaken in Germany in 2015. There is an obvious 'skew' in the distribution. We can see that only 11.8% of the sample had a blood vitamin D greater than 75nmol/L, which is 30ng/ml. More than half had a blood level less than 50nmol/L, which is only 20ng/ml.
The solid red line represents the threshold: research during the pandemic has shown us that lower vitamin D levels are associated with a increased risk of serious Covid-19m whereas above this threshold the risk of serious illness is very low.
The dotted red line represents 100nmol/L, which is 40ng/ml. This should be the safe target blood level.
A recent study in Israel observed 1176 people admitted hospital with Covid-19 and of whom 253 in retropect were found to have records of previous blood levels of Vitamin D.
 |
| Figure 3. Blood levels of Vitamin D in Israel |
Once again we find that half the group of patients had blood levels of Vitamin D less than 20ng/ml, 50nmol/L.
The serious disadvantage of Vitamin D deficiency
I have reviewed the findings of this study from Israel in a previous Blog post. If we look at the patients who were critically ill with Covid-19 we can see a summary of the findings of the study.
 |
| Figure 4. Blood levels of VItamin D predicting severity of Covid-19 |
It shows what previous studies had shown, that patients with critical or fatal Covid-19 almost entirely had low levels of Vitamin D. We can also judge the blood level of Vitamin D that appears to be 'safe', like a safe blood pressure or glucose. This can only be judged by careful observation, as in Israel. The role of observation has been repeatedly trivialised during the pandemic (apart from in vaccine assessments), but science is based on careful observation.
Observation tells us that a blood Vitamin D level above 30ng/ml, 75nmol/L, is perfectly safe and reduces considerably the risk of critical or fatal Covid-19. To aim at the range of 40 to 60 ng/ml, 100 to 150 nmol/L is wise, to make certain that we have a full reserve. Various studies, including that from Israel, have shown no cases of Vitamin D excess.
We can also see from the study in Israel that very few people have a blood level of Vitamin D greater that 30ng/ml, 75nmol/L, despite living in a very sunny country. Vitamin D deficiency is very common, 50% in this sample, remembering that the blood testing was well in advance of the illness.
The present definition of Vitamin D deficiency
Vitamin D deficiency should be defined as a blood level less than 30ng/ml, 75nmol/L. It has previously been defined as less than 10ng/ml, 25nmol/L but this was based on the prevention of rickets, not on optimisation of immunity and protection against serious infection. As mentioned above SACN, the UK Standing Advisory Committee on Nutrition, does not acknowledge the pivotal role of Vitamin D in defensive immunity, just mentioning that there is a 'suggestion'. I hope that during the pandemic of Covid-19 SACN has learned as much about the importance of Vitamin D as I have learned.
There is sometmes the expression of 'Vitamin D insufficiency', meaning somewhere between deficiency and adequacy or ideal. 'Insufficiency effectively means little reserve, a situation best avoided if possible, whether Vitamin D, fuel in the car, money in the bank. When setting out on a car journey it would be unwise to have an insufficiency of fuel.
I have used the analogy previously of the motor car and the importance of a full tank of petrol or diesel, or a full battery charge, when setting out on a long and uncertain journey. And so it is with Vitamin D during our uncertain journey through life: we do not want to 'conk out' on the way, before reaching our expected destination.
The need for a constant supply of VItamin D
It is important that we have a fairly constant supply of Vitamin D so as to maintain the reserve of 25(OH)D, calcifediol, in the blood. This is difficult when we live closer to the North Pole than to the Equator, and especially with indoor work. Solar UV has little opportunity to produce Vitamin D in our skin.
We have seen that in temperate zones serious Vitamin D deficiency is common and serious illness can result from it. In the interests of the health of the public it would be sensible to screen for blood levels of Vitamin D and correct with appropriate supplement if deficient. Screening should certainly occur early in pregnancy so that no baby is born with Vitamin D deficiency.
This is the ideal but before we get to that point, a 60kg person living in temperate zones should take a supplement of Vitamin D 3,000 units daily, scaled up or down depending on body weight. Even if you are not deficient, taking this will be of no disadvantage.
 |
| Winter sun at 45 degrees north of the equator, but no Vitamin D production |
