 |
| London – Greenwich and Canary Wharf |
It has been established very well during the Covid-19 pandemic that a low blood levels of Vitamin D recorded in advance of illness (Santander, Heidelberg, Israel ) is the most significant but potentially reversible risk indicator of critical disease and death. Vitamin D deficiency is also the common factor within the major at-risk groups, the obese, the elderly, and those of South Asian and Black African ethnicity who live in the UK and other northern European countries.
It has been established that Vitamin D in its "raw" form when given to the critically ill in Intensive Care Units (ICU) is not effective (Brazil), the simple reason being that as we know, it takes up to two weeks for the Vitamin D to be converted in the liver into its hydroxylated pre-active form, 25(OH)D, also known as Calcifediol. When Calcifediol is given by mouth it takes just two hours to achieve good blood levels. It is Calcifediol, 25(OH)D that we measure in the blood as Vitamin D.
Randomised controlled trials (Cordoba and Barcelona) have shown that when Calcifediol is given to patients admitted to hospital on account of severe Covid-19, it is remarkably successful in reducing the risk of escalation to ventilatory care and death. Why it has not been used widely in the UK and elsewhere is a mystery.
Correction of vitamin D deficiency
It would be a sensible public health initiative to correct Vitamin D deficiency within the population, especially in those at particular risk. A "safe" level of Vitamin D in the blood should be achieved, ideally before admission to hospital. Vitamin D is cheap, readily available, and safe when given in physiological doses checked by blood levels.
It is clear that a low blood level of vitamin D (=Vitamin D deficiency) can be a serious disadvantage, and restoration to an ideal blood level of 40ng/ml (100nmol/L) would be sensible. But how to achieve this is the challenge.
The physiological way to obtain Vitamin D is by exposure of the skin to the sun, at times when at close to sea level the sun is more than 45 degrees above the horizon, judged by the length of the shadow being less that the height. This could be recommended but an excessive single exposure leading to burn is to be avoided.
It has been demonstrated that not only people with ideal blood levels of Vitamin D have a reduced risk of critical or fatal Covid-19, but also people who are taking vitamin D supplements at the time of hospital admission on account of Covid-19 (Tameside, UK).
The biology of the pivotal role of Vitamin D, in its fully activated form 1,25(OH)D, in the escalation of natural defensive immunity has been established during the past forty years.
With the onset of a serious pandemic due to a new respiratory virus, it would seem to be sensible to act on a knowledge of medical science supported by early reports of the dangers of low blood levels of Vitamin D. Correcting Vitamin D deficiency would have been of great potential benefit, with no danger. I have drawn attention to the report of just a single case of vitamin D toxicity occurring during the pandemic.
Randomised controlled trial – RCT – from UK
Official advice concerning the use of Vitamin D during the pandemic was very negative, ridiculously so given the circumstances and 200,000 Covid-19 deaths in the UK. The pandemic emergency resulted in vaccines being issued on the basis of Emergency Use Authorisation (EUA), meaning that only short term and rudimentary RCTs in healthy people had been completed.
When it came to vaccinations in pregnancy there were no RCTs, which can be regarded as negligent. Safety was to be judged on the basis of "post–marketing surveillance". And this is the important thing: the main purpose of RCTs is to establish safety, following the thalidomide tragedy of the 1960s. When taking medicines, effectiveness is less importance than safety. A medicine might not do good, but it must not do harm – primum non nocere.
Whereas the "vaccines" against Covid-19 are a new RNA technology with safety being far from clear, Vitamin D is a natural substance that has been in use for a century. The standard dose range is known, with appropriate blood levels. The exceptionally rare side-effect of Vitamin D intoxication (hypervitaminosis D) is always the result of major dose error and is both easily recognised and completely reversible. The need for RCTs of Vitamin D was much less pressing than for vaccines.
The challenge of prospective randomised trials of vitamin D, or anything else, is that if low-risk individuals are to be studied, very large numbers must be recruited if the endpoint of critical illness or death is to be reached in significant numbers. Administration costs are inevitably very high, and follow-up times will be long. It imight be sensible to concentrate on a smaller number of individuals who are at high risk of serious or fatal Covid-19. Hence the success of the RCTs from Spain, small numbers showing a big effect with statistical significance.
I have also shown in previous Blog posts the wisdom of Sir Austin Bradford Hill, whose criteria of pragmatic "proof" (it is never absolute) identifies an RCT as being only one component. For ethical and operational reasons an RCT might not be possible, or be of only limited value. There is also the wisdom of Blaise Pascal, who realised that decision-making is also pragmatic, a trade-off between likely benefit and possible adverse outcome.
United Kingdom - the COVIDENCE UK study
Early in the pandemic in the UK, a large community-based clinical trial of Vitamin D in the prevention of Covid-19 was proposed by Professor Adrian Martineau. Funding of the study became an immediate problem as a large administrative staff would be essential and there would be no pharmaceutical company support. However the study was undertaken and the result became available in early 2022.
6200 adults were incorporated into the trial, with a number of exclusion criteria including current Vitamin D supplementation. 2958 of these were randomised to receive Vitamin D.
2690 (86.8%) of those to receive VItamin D had blood Vitamin D levels less than 30ng/ml, 75nmol/ml. This shows the extent of clinically significant Vitamin D deficiency. They had suboptimal blood levels as identified in the observational studies described in Heidelberg, Israel, and other places.
1334 were given a lower dose of vitamin D supplement, 800 units per day, and 1356 were given a higher dose, 3200 units per day.
The controls did not have blood testing and they were informed that they were not to receive a Vitamin D supplement. This is important as, with the Heidelberg and Israel studies, the identification of Vitamin D deficiency before the study would have created the ethical dilemma if they were not to have the deficiency corrected.
There was no placebo given to the control group. This weakened the trial and in the knowledge that they were not to receive Vitamin D that was being tested, the controls would be likely to take a Vitamin D suplement not given to them. In fact 49.9% of them did so on at least one occasion.
The trial commenced in December 2020, with six month follow-up of individuals. The vaccination process was under way at that time and 89.1% of the subjects received one or more doses of a Covid-19 vaccination during the study period. This would obviously complicate the interpretation of the results.
The baseline Vitamin D levels can be seen in Figure 1. Both units in current use are shown, nmol/L and ng/ml. We can see no significance difference between the two treatment groups at the baseline. We see again the high prevalence of low sub-optimal blood levels of Vitamin D.
 |
| Figure 1. Baseline blood levels of Vitamin D |
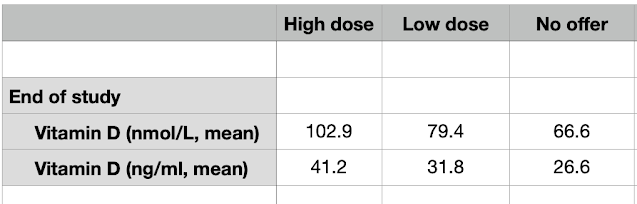 |
| Figure 2. End of study blood levels of Vitamin D |

