When the pandemic of Covid-19 emerged two years ago, those medical scientists with a knowledge of the importance of defensive immunity realised that the most immediate and important action must be the correction of Vitamin D deficiency, which is found in the majority of the population.
Research during the previous forty years had worked out the details of the escalation of defensive immunity in response to infection, information that was not available in the previuos major pandemics of infuenza. The new information involved the vital role of Vitamin D, in its activated form 1,25(OH)D. It was also known that Vitamin D deficiency is very common in the UK and other European countries. It had been established that Vitamin D deficiency is particularly common and severe in certain groups such as the elderly, the obese, people with diabetes or malignancy, and people of South Asian and Black African ethnicity living in Europe. All such groups had a high mortality rate from Covid-19.
Despite advice from independent scientists, those not employed directly by governments, Vitamin D was ignored. The government policies in the US and UK (and elsewhere) were for vaccines to be developed to control Covid-19 infections and for no natural preventative or known pharmaceutical interventions to be considered.
Deaths from Covid-19
It was not long before Covid-19 caused large numbers of deaths, but those who had died had been offered no immunological protection. Medical scientists who knew of the importance of vitamin D deficiency at this time of pandemic brought this to national attention, but they were ignored. Our political, medical, and public health leaders denied the importance of Vitamin D in the process of immunity. We were perpetually told that there was no evidence that Vitamin D would help in the treatment of Covid-19. Of course there was no specific evidence for the simple reason that the virus was new. We could say the same about vaccines.
But there was good evidence that optimisation of immunity would be an advantage in face of a pandemic, and that Vitamin D is vital for that optimisation. I have pointed out Pascal's Wager, that in the absence of conclusive information (eg the existence of God, or the benfit of Vitamin D in Covid-19) it is important to take the line of least damage and maximum potential benefit. The potential benefit of Vitamin D is far greater than any significant disadvantage, as judged by experience gained during many decades of use. After all, the idea would be to correct deficiency of a natural vitamin/hormone, not to introduce a new and barely-tested medicine.
The denial of VItamin D
Has it been ignorance or ignoring?
Our national officials continued to deny the potential benefits of Vitamin D. They continued to advise witholding VItamin D for immunity optimisation until "proof" of benefit had been demonstrated in a randomised controlled trial (RCT). They seemed to be unaware of the meaning of "proof", and unaware of the serious limitations of an RCT (cost, ethics, logistics). It was obvious that there would be many Covid-19 cases, hospital admissions, and deaths while an RCT would be planned, undertaken, analysed, published, and debated. The realisation of emergency was demonstrated by the introduction of injected mRNA (aka vaccination) given after only rudimentary clinical testing, but natural Vitamin D cheap, safe, and readily available was not allowed.
From May onwards in 2020 nature provided a predictable respite from Covid-19 as the result of the natural summer-time production of Vitamin D, but even this was not officially recognised. Was it ignorance or deliberate ignoring of Vitamin D? Our medical-scientific leaders should not have been ignorant of Vitamin D and its importance in immunity, but supression of that information was essential for the emergency use authorisation (EUA) that would allow the release of new and barely tested "vaccines".
As the pandemic progressed we received a great deal of information concerning the importance of low blood levels of vitamin D in the devlopment of critical and fatal Covid-19, protection by good blood levels (40–50 ng/ml, 100-125nmol/L). The evidence in favour of an important and readily available role for vitamin D in safely minimising the impact of the pandemic has been consistently ignored or suppressed.
Information concerning the importance of vitamin D has continied to accumulate, recently from Belgium and Mexico, and most recently from the USA.
Evidence for the USA
Important evidence became available on November 12th 2022. The study came from the Department of Veterans Affairs (VA) health network in the USA. It was a retrospective cohort study, with the title "Association between vitamin D supplementation and COVID-19 infection and mortality". The authors were from a variety of important medical and university institutions in the USA.
The study identified the records of veterans of the US armed forces, who had blood tests and/or prescriptions for vitamin D between January 1st 2019 and December 31st 2020, which is before vaccines were introduced.
34,710 had received a prescription for vitamin D2 (of fungal origin) and 220,265 had received a prescription for vitamin D3 (of animal origin, usually from the oils of sheep's wool). 407,860 controls were identified (no vitamin D supplement taken).
The study objectives were to calculate the time to Covid-19 infection, and the mortality within 30 days of infection.
For the purpose of the study 33,216 subjects treated with vitamin D2 (average age 58) were carefully matched with 33,216 controls (average age 58). 220,265 subjects treated with vitamin D3 (average age 64) were matched with 407,860 controls (average age 63). The details of the matches are shown in the paper.
In the vitamin D3 group, there were 359,091 men and 39,915 women, 71,071 Black and 283, 248 White subjects.
VItamin D results
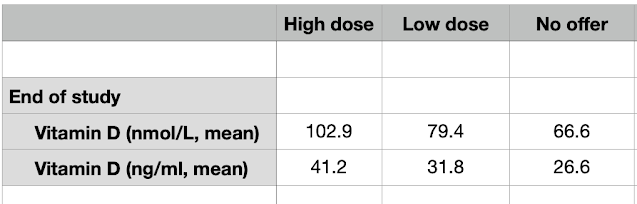
For the vitamin D3 group, the Vitamin D blood level results before the pandemic are as follows:
 |
| Figure1. Blood levels of Vitamin D in the subjects of the USA VA study. ng/ml and nmol/L |
Experience in other observational studies indicates that the risk of critical or fatal Covid-19 is extremely low when the blood level of vitamin D is at or greater than 40 ng/ml, 100 nmol/L. Other studies have show that only about 15 – 25% of people fall into this range. In this present VA study only 25% of the 399,006 subjects had a "good" level of vitamin D, 75% being deficient, and 17% being very deficient with high Covid-19 mortality risk.
Men were found to have on average lower blood levels of vitamin D compared to women.
Black subjects tended to have lower blood levels of Vitamin D and higher rates of Covid-19 infection.
The group taking vitamin D2 was too small for detailed analysis.
The dose of Vitamin D taken had a very wide range, from 20 units per tp 15,000 units.
Outome assessment
There were clear advantages in those taking Vitamin D supplements compared to untreated controls, as shown in Figure 2. The results are displayed as hazard ratios (HR), the control risk being standardised as 1.0 and the Vitamin D treated groups a lower number indicating benefit (lower infection or death rates).
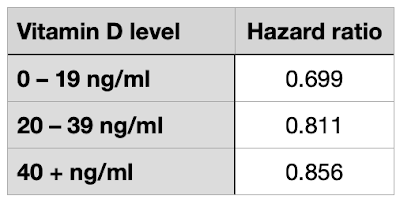 |
| Figure 2. Hazard ratios for Covid-19 infection based on blood levels of Vitamin D (lower HR greater risk) |
For Vitamin D3 treated subjects, the HR for Covid-19 infection is 0.797. For Vitamin D2 treated subjects, the HR for Covid-19 infection is 0.720. The benefit is shown clearly in the bar chart of Figure 3. The outcome for those taking D2 was slightly better than those taking D3, but there was a risk reduction of 25 – 30% for both groups. A clear benefit.
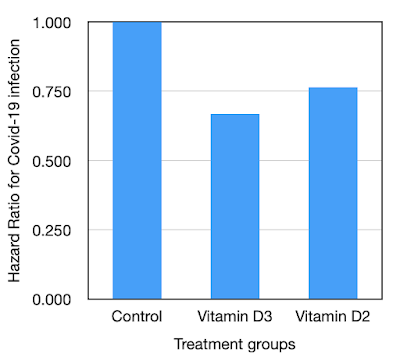 |
| Figure 3. Hazard ratios for Covid-19 infection for Vitamin D3 and D2 |
In Figure 4 we can see that for Vitamin D3 treated subjects, the HR for death within 30 days of Covid-19 infection was 0.667. For Vitamin D2 treated subjects the HR for death within 30 days of Covid-19 infection was 0.765. The outcome for those taking Vitamin D3 (the great majority) was significantly better than for those taking Vitamin D2.
 |
| Figure 4. Hazard ratios for death within 30 days of Covid-19 for Vitamin D3 and D2 |
For the subjects taking Vitamin D3, the risk reduction for death within 30 days of Covid-19 infection is 33% compared to controls. This a major benefit.
Further information is given in the paper.
The analysis was based on medical records. No toxic effects of Vitamin D were recorded.
The greatest benefit was seen in the subjects with the most severe Vitamin D deficiency, less than 20ng/ml, 50nmol/L. Vitamin D supplement of 50,000 units per day brought about an infection HR of 0.51, which is a 49% reduction of Covid-19 infection risk. This is a great short-term benefit but the dose is very high for long-term use.
The risk reduction for Covid-19 infection in men and women was similar, HR 0.8 in men and HR 0.77 in women, corressponding to 20% and 23% risk reduction respectively.
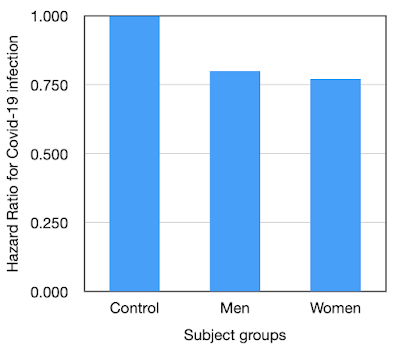 |
| Figure 5. Hazard ratios for Covid-19 infection men and women |
Risk reduction was greater in Black subjects compared to White.
 |
| Figure 6. Hazard ratios for Covid-19 infection Black and White subjects |
The respective HRs indicate a 30% risk reduction for Black subjects receiving a Vitamin D supplement comared to a 20% risk reduction in matched White subjects. This probably represents initially lower blood levels of Vitamin D in the Black subjects.
Vitamin D: blood levels and supplements.
The USA VA study was retrospective controlled. The variables of initial blood levels of Vitamin D and the dose of Vitamin D supplement were recorded. They were only linked when the analysis was undertaken. The supplements, with a wide range of doses, were not necessarily based on blood levels at the time of prescription.
It might be expected that those with good blood levels of Vitamin D would not need or be given a supplement, but in practice many were. The results of the study indictate that those with initial very low blood levels of Vitamin D benefited more than those with good blood levels. However those with good blood levels (40ng/ml, 100nmol/L or greater) also benefited. Risk reductions are shown in Figure 7.
 |
| Figure 7. Risk reduction from Vitamin D based on initial blood level of Vitamin D |
However, the subjects that would not be considered to be Vitamin D deficient experienced a 14% risk reduction when given Vitamin D supplements. This suggests that in advance of a pandemic, giving a Vitamin D supplement to all people would be of considerable advantage, without needing to test for blood levels until later.
Conclusions
This is yet another study that has shown the disadvantage of low blood levels of Vitamin D, and the great medical/biological advantage of correction with a Vitamin D supplement.
How long can our major media, medical scientific, public health, and political leaders continue to ignore and deny the great importance of and benefits from Vitamin D?
From February 2020 onwards many cases of and deaths from Covid-19 could have been prevented if the pre-existing knowledge of the importance and safety of Vitamin D had been been put into action. Of course there was no pre-pandemic experience of Vitamin D supplement in respect of Covid-19, but action could have been taken, the application of Pascal's wager. There was too much demand for "proof" and "more evidence" from people who could not understand the nature of proof.
The authors state: "When we extrapolate our results for Vitamin D3 supplementation to the entire US population in 2020, there would have been approximately 4 million fewer Covid-19 cases and 116,000 deaths avoided".
If only.....
But for the next pandemic there is official prediction only for more mRNA vaccines, but no mention of Vitamin D, despite all the evidence of effectiveness and safety.