Covid-19 and Vitamin D – a study from Liverpool
 |
| Liverpool water-front |
We have just seen the publication of another paper concerning the outcome of Covid-19 in relation to the blood level of Vitamin D. This study was undertaken in Liverpool, UK.
The results are not entirely straightforward as the study also investigated several parameters of Vitamin D. I will try to extract what I regard as the most important points and integrate them with other studies.
The study was of 992 patients with Covid-19 admitted to hospital in Liverpool between March 18th and November 2nd 2020, early in the pandemic. Of these, 472 were studied in detail because following initial blood testing, there was sufficient surplus blood serum to allow retrospective blood testing for Vitamin D.
Vitamin D levels
From the recent study from Israel, I find it compelling that Vitamin D deficiency should be defined as less than 30ng/ml, 75 nmol/L. Less than this blood level indicates a high risk of severe or critical Covid-19, whereas above this level can be regarded as a safe range. In the study from Israel about 50% were deficient by this definition, and in a study from Heidelberg, Germany, in 2020 the proportion deficient of Vitamin D in was much higher at about 80%, in Figure 1.
 |
| Figure 1. Vitamin D in patients with Covid-19, 2020 |
In my personal research in Blackburn, UK, 20 years ago the proportion with Vitamin D deficiency as defined above using the Israel data, was 682 in the ethnic white sample of 818 (83%), and a very disturbing 1514 in the ethnic South Asian group of 1574 (96%).
I have shown this data previously, but as it was two years ago I will display the bar-charts below. Each vertical bar represents the blood vitamin D level of one person. As the distribution is not "normal" or symmetrical, the median is shown. This is the halfway point, 50% of the subjects below or above this level, the vertical orange line. The horizontal yellow line indicates the blood level of the median. The horizontal red line indicates blood vitamin D level of 30ng/ml, 75nmol/L and we can immediately see how few of the subjects were above this safe line.
 |
| Figure 2. Distribution of blood level of Vitamin D in 818 ethnic white people |
 | |
|
Liverpool experience
Once again we have the problem of two units of measurement of Vitamin D in current use. The paper from Liverpool uses the unit "nmol/L". I will express both even though this might appear cumbersome. 1ng/ml = 2.5nmol/L
The Liverpool study regarded 20ng/ml, 50nmol/L as being the lower limit of the ideal range, and therefore below this to be VItamin D deficiency. However the study from Israel indicated that 30ng/ml, 75 nmol/L would better be regarded as the lower limit of the safe range, based on biological advantage.
Of the 472 Covid-19 patients studied in Liverpool, we can see in Figure 4 the numbers with various blood vitamin D levels.
83% were deficient of Vitamin D with blood levels less than 30ng/ml, 75nmol/L.
The pattern is similar to but not quite as dramatic as the Heidelberg study ahown in Figure 1. In this, there are more sub-divisions of Vitamin D level than in Figure 4.
Deaths
Of the 472 Covid-19 patients, 112 died within 28 days, 23.7% overall, 28% in men, 23.5% in women. This proportion of deaths was the general experience during 2020, when the highly vulnerable members of the population died.
Of those who died:
Average (median) blood level of vitamin D was 15.8ng/ml, 39.5nmol/L.
Of those who survived:
Average (median) blood level of vitamin D was 17.3ng/ml, 43nmol/L.
Those who survived had on average a slightly higher blood vitamin D level than those who died, in keeping with other studies, but the difference was not dramatic. The difference did not achieve "statistical significance", meaning that it could have been a chance finding. Whether or not there is clinical significance is a matter of judgement, a balance of potential benefits and risks of using or not using Vitamin D in clinical practice.
Statistical significance is influenced to a major extent in sample size. In investigating the effect of Vitamin D in Covid-19, it is operationally difficult to use a large sample size, unlike a pharmaceutical trial in a sample of normal people in the community.
More detail is shown in Figure 5. Look at it carefully to see which green columns (died) were higher than the blue (survived).
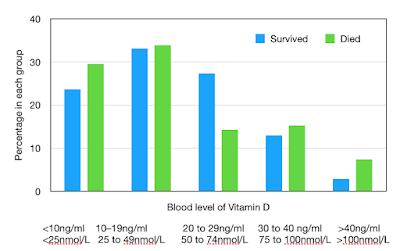 |
| Figure 5. Covid-19 survival or death and Vitamin D |
We can see that the chance of death is greatest in those with the lowest blood levels of VItamin D, but also in those with the highest.
Severe disease
The infuence of Vitamin D on severe Covid-19 was expressed as Odds Ratio, the relative chance of developing severe Covid-19 based on blood level of Vitamin D. The reference was a blood level of 20–30ng/ml, 50–74 nmol/L, as considered to be middle of the range found in the general population.
The odds ratio for severe disease:
for Vitamin D 20–30ng/ml, 50–74 nmol/L OR=1 (reference)
for Vitamin D <10ng/ml, <25nmol/L OR=2.37
There is no surprise here: severe disease is much more likely in those with the the very low blood levels of VItamin D, less than 10ng/ml, 25nmol/L.
The study therefore identified something expected. But there is more to consider.
High blood VItamin D
There were 18 patients with Vitamin D greater than 40ng/ml, 100nmol/L. For these the odds ratio of severe Covid-19 was high, with OR=4.65. This was an unexpected finding.
We know about Vitamin D "intoxication", hypervitaminosis D, in which excess Vitamin D causes an increase in the amount of calcium in the blood and in the urine. This can occur only with very high blood levels of Vitamin D, greater than about 200ng/ml, 500nmol/L.
But in this study there was no hypervitaminosis D, as judged by high calcium level in the blood, but we do see a disadvantage of a blood Vitamin D level just greater than 40ng/ml, 100nmol/L.
The report is of quadruple (OR=4.65) the risk of severe Covid-19 in this group with Vitamin D level >40ng/ml, 100nmol/L compared to the reference range of 20–30ng/ml, 50–74 nmol/L.
An explanation
This finding came as a surprise to me as this result has not appeared in other studies. Is it just a chance finding, a sort of mistake? All findings need to be replicated before they are generally accepted, or there must be a plausible mechanism, some connection that makes sense. But initial findings such as this must not be dismissed.
The paper from the study looked into a plausible explanation.
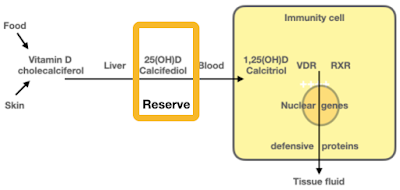
We must remember that Vitamin D produced in the skin or taken by mouth must be converted in the liver into 25(OH)D, the form which it circulates in the blood.
In response to infection and to enable immune response, 25(OH)D is taken up by the immunity cells and is activated into 1,25(OH)D, which then unlocks VDR. A molecule of 1,25(OH)D can be used only once, and then it is converted into the inactive 24,25(OH)D.
25(OH)D is converted into the active 1,25(OH)D by the enzyme 1-alpha hydroxylase. Now, it appears that when the blood level of 25(OH)D increases above 40ng/ml, 100nmol/L, "Fibroblast Growth Factor 23" (FGF23) is induced, and this leads to the suppression of the enzyme 1-alpha hydroxylase. Activation of 25(OH)D to 1,25(OH)D will thereby be suppressed, and as a result there will be a diminished immune response.
This is a perfect example of the interaction of enzyme systems, feedback control mechanisms, that became essential in evolution. The inactivation of 1,25(OH)D to 24,25(OH)D is an excellent example of an essential control system, and the suppression of the enzyme 1-alpha hydroxylase would be another.
Free and bio-available Vitamin D
Other Vitamin D parameters were investigated in the Liverpool study. When we assess blood levels of Vitamin D we measure it in its form that has been processed in the liver, 25(OH)D (also known as calcidiol or calcifediol). This is carried in the blood as a reserve, ready for use as and when necessary. In the blood it is bound to a specific Vitamin D Binding Protein (DBP), the amount of which can vary from person to person. This is because DBP is genetically determined, and the gene penetration is variable, determined by genetic polymorphisms, differences. The vast majority of 25(OH)D is bound to DBP and only 0.03% of it "free", unbound. Did this make a difference?
This was investigated and it was found that there was no relationship between DBP, and free D with mortality. Measuring 25(OH)D seems to be a satisfactory way to assess Vitamin D status.
Conclusion
The pandemic of Covid-19 has given huge research opportunity to investigate the optimisation of natural defensive immunity, with the role of Vitamin D based on extensive research during the previous forty years.
Taking together the Israel and Liverpool studies, we can conclude that to minimise severe or fatal Covid-19 it is necessary for the blood level of Vitamin D to be between 30ng/ml, 75nmol/L and 40ng/ml, 100nmol/L.
It is clear that it is necessary to monitor regularly the blood level of Vitamin D so as to determine the optimal dose.
We must monitor the blood parameters when correcting Vitamin D deficiency just as we monitor blood parameters when we treat diabetes and thyroid disorders.
I have noted many Comments. I have attempted to reply to them, but unfortunately, and for reasons that I do not understand, my replies do not attach. Sorry about this.

Many thanks for this - it's really interesting.
ReplyDeleteYou would think that every health centre in the country would now be adding vit D level to every routine blood test, but in my own case I have only experienced resistance when I've asked for it.
It seems the NHS is happy to blow a fortune on covid jabs & nosebags, but unwilling to invest in low cost & more effective preventative measures. Why is this?
DevonshireDozer
This appears to be the only study where a level higher than 40ng/mL seems to confer a disadvantage. Also it has not got a very large number of participants. Given that more than one of the other studies has shown that levels above 50 or even 55ng/mL result in virtually zero deaths from covid might it not be that there are some as yet unidentified confounders at work in these patients and that their higher vit D levels were incidental? Perhaps it would have been better if calcitriol levels were monitored as well as calcifediol.
ReplyDeleteAgreed
DeleteIs there any room for reverse causality? That is, were the small number in the higher range taking vitamin supplements due to existing health issues? Given this is England, having greater than 100nmol/l would require an exceptional diet or sun exposure if not supplementing.
DeleteWell what are those of us to do who have vitamin D levels above 100nmol/L ? Mine's been around what was called optimal levels of 150nmol/L for years ! I don't seem to get infections very easily either. Since it's just this Liverpool study which has shown that levels above 100nmol/L aren't good why not defer to other studies ?
ReplyDeleteYes it's only one study. To date the only recognized adverse events associated with Vitamin D toxicity are hypercalcemia and hypercalcuria. It does however, again confirm that inflammation is associated with severe Covid symptoms. In this case elevated CRP and decreased GFR may indicate kidney inflammation and reduced ability to make calcitriol. The 'ACKNOWLEDGEMENTS' section seems to be in lieu of a conflicts of interest statement.
DeleteAs you say this is another vote for vitamin D supplementation to cure the deficiency that you have noted in many people in your medical career. I hope it inspires more physicians to look at environmental factors in disease.
ReplyDeleteI find it hard to believe that a calcifediol levels > 40 ng/mL is deleterious in itself because it is easy to get to 60 ng/mL just by being in the sun. Evolution would have done something about that!
The confounding factors may be vitamin K2 and magnesium.
My own recommendation is to take D3 with K2 and a magnesium supplement.
K2 is another vitamin in which many people are deficient [1]. Low K2 will lead to arterial calcification as the D makes calcium available and K2 gets it from blood into bone.
However, I think magnesium deficiency is a more likely factor. Magnesium is an important element in our system [2]. Vitamin D3 uses magnesium. The higher the serum D, the more the magnesium will be depleted with serious health consequences.
As you can see from the articles both K & magnesium deficiency cause cardiovascular problems. As sars-cov-2 also causes vascular problems, it compounds the problem.
1) A useful summary of the K vitamins and deficiency: Vitamins K1 and K2: The Emerging Group of Vitamins Required for Human Health, https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC5494092/
2) A useful summary of magnesium and deficiency: Subclinical magnesium deficiency: a principal driver of cardiovascular disease and a public health crisis, https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC5786912/
I wrote the comment above asking what should those of us do who have what is considered optimal levels of D, mine around 150nmol/L for many years (apart from ignoring the Liverpool result). I do take vitamin K2, been taking that for years too. I don't take magnesium supplements as it upsets my gut badly, no matter what form of magnesium - I read that if that happens it indicates one is getting enough magnesium and one doesn't need supplementation - I'd be interested to know more.
DeleteI never heard that gastric/gut upset from magnesium supplements implied one had an adequate amount. Magnesium glycinate is the easiest on the gut. Best to get your blood Mg checked though it is unlikely to be too much unless you have failing kidneys. Less than 1% of magnesium is in the blood.
ReplyDeleteThanks, I'll try magnesium glycinate. I do have a very good diet, high fat, low carb, no processed foods either. I probably don't have magnesium deficiency though.
Delete